Imagine Marie, a mother of two juggling her family responsibilities with her full-time job. After several months of intense pressure and stress, she begins to experience more worrying symptoms: frequent infections, persistent colds and slow healing of small wounds. When she consulted a therapist, he explained that her condition could be linked to a dysfunction in her immune system, exacerbated by the chronic stress she was under. Indeed, prolonged stress can weaken the immune system, making the body less able to defend itself against infection. This situation perfectly illustrates the importance of understanding the relationship between stress and the immune system, a subject that deserves our attention, especially for massage therapy practitioners.
| Contents: Stress and the immune system: a complex link The impact of inflammation on mental health Approaches to better managing stress and inflammation Towards a better understanding Conclusion |
Stress and the immune system: a complex link
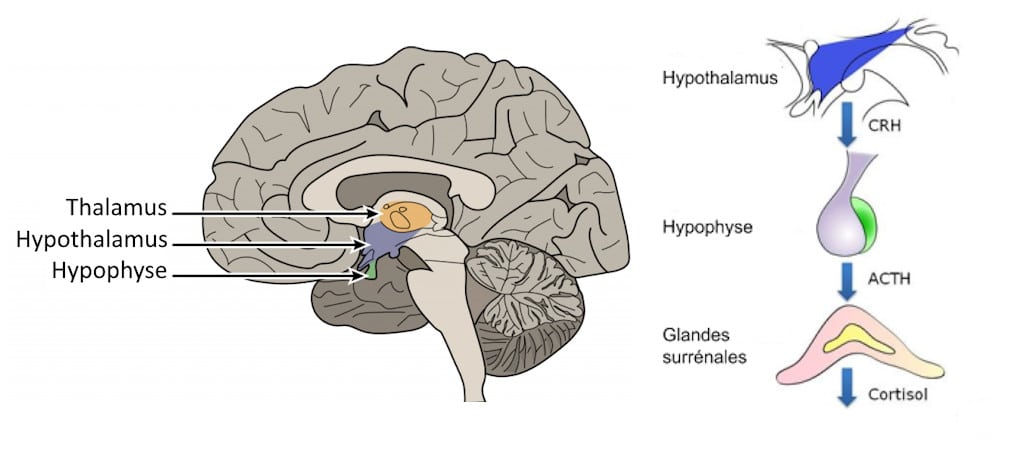
Stress activates biological responses that modify our state of health. When faced with a stressful situation, the body reacts by activating the hypothalamic-pituitary-adrenal (HPA) axis and the sympathetic nervous system. The HPA axis begins with the hypothalamus, a region of the brain that detects stress and releases a hormone called corticotropin (CRH). This hormone stimulates the pituitary gland, located just below the hypothalamus, to secrete adrenocorticotropic hormone (ACTH). In turn, ACTH stimulates the adrenal glands to produce glucocorticoids, including cortisol, a hormone that plays a crucial role in stress management. Cortisol helps modulate inflammation and regulate various metabolic processes such as circadian rhythm, and enables a rapid response to stress.
In situations of chronic stress, prolonged overactivation of noradrenergic neurotransmitters leads to resistance to glucocorticoids, disrupting their anti-inflammatory action and promoting an intensification of inflammatory processes in the body. This imbalance can have serious consequences for mental and physical health, leading to mood disorders such as depression and anxiety.
The impact of inflammation on physical and mental health
Research has shown that inflammation plays a central role in the manifestation of mood disorders. Inflammatory markers, such as pro-inflammatory cytokines, are often present at high levels in individuals suffering from depression or anxiety. These molecules can alter neurotransmitter transmission and affect the way our brains regulate our emotions. Thus, an inflammatory state can reinforce vulnerability to stress and aggravate the symptoms of mood disorders. Marie’s chronic fatigue and irritability may be indicators of anxiety or depressive disorders.
Inflammation can also affect other systems in the body. It is linked to chronic diseases such as cardiovascular disease, type 2 diabetes and certain autoimmune disorders. Prolonged inflammation can upset the balance of immune cells, which can compromise the body’s ability to fight infection and repair itself. Consequently, an integrative approach that considers both mental and physical health is essential to promote well-being.
Approaches to managing stress and inflammation
Stress management practices such as meditation, deep breathing, massage and exercise play an essential role in coping with stress. These activities help to regulate the immune response and, combined with a balanced lifestyle including a healthy diet and good sleep, contribute to lasting well-being. By integrating these approaches, therapists can not only help their clients relax, but also make them aware of the crucial impact of good stress management on their physical and mental health.
In short, the link between stress, the immune system and inflammation is complex and multifaceted. By understanding these interactions, massage practitioners can play a key role in improving their clients’ well-being, providing them with tools to better manage stress and promote optimal health. The relationship between stress and the immune system is a growing area of research. Studies suggest that improving our understanding of these mechanisms could pave the way for more personalized and effective treatments for mood disorders. As massage therapy practitioners, it’s essential that we keep abreast of advances in this field and adapt our practices to meet our clients’ needs.
Conclusion
By learning to manage her stress through massage and other techniques, Marie can look forward not only to improving her mental well-being, but also strengthening her immune system. By understanding the complex relationship between stress and inflammation, she is empowered to take care of her health.
To remember:
- Stress activates the HPA axis, leading to the production of cortisol, a key anti-inflammatory hormone.
- In the long term, cortisol becomes less effective, promoting inflammation and imbalances in the body.
- Physical and mental health : Chronic inflammation is linked to mood disorders and diseases such as diabetes and cardiovascular disease.
- Massage, meditation and exercise as relaxation interventions help to reduce stress, regulate inflammation and improve overall well-being.
Sources :
- Hassamal, S. (2023). Chronic stress, neuroinflammation, and depression: an overview of pathophysiological mechanisms and emerging anti-inflammatories. Frontiers in Psychiatry, 14. https://doi.org/10.3389/fpsyt.2023.1130989
- James, K. A., Stromin, J. I., Steenkamp, N., & Combrinck, M. I. (2023). Understanding the relationships between physiological and psychosocial stress, cortisol and cognition. Frontiers in Endocrinology, 14. https://doi.org/10.3389/fendo.2023.1085950
- Tong, R. L., Kahn, U. N., Grafe, L. A., Hitti, F. L., Fried, N. T., & Corbett, B. F. (2023). Stress circuitry: mechanisms behind nervous and immune system communication that influence behavior. Frontiers in Psychiatry, 14. https://doi.org/10.3389/fpsyt.2023.1240783

